According to the Office of Inspector General your hospital may be on the hook for implant recall reporting after they found more than 900 hospitals failed to reimburse $33M to the Centers of Medicare and Medicaid Services (CMS) for credits associated with recalled implants. Ensuring your facility’s implant recall management process is compliant with CMS regulations is critical to minimizing the risk of OIG exposure and ensuring patient safety.
For many hospitals, managing the implant recall process presents challenges around communication and coordination. Further, it is imperative to understand your obligation to CMS and other Federal entities.
What needs to happen when a recall is issued?
- Identify if recalled products are being held in existing inventory and sequester any affected products
- Submit the recall response form to the recall initiating manufacturer or vendor
- Identify patients affected, including when, where, and who were potentially exposed to the recalled medical devices
- In certain cases, notify surgeons and patients potentially exposed to recalled medical devices or implants
- Issue required credits for cases involving Medicare and Medicaid patients for both government and privately plans
- Issue credits to other payors based on the requirements of federal regulations
What are the obstacles to your timely compliance?
- Not enough resources or staff familiar with your enterprise IT systems to compile required data and the inability to fill in gaps in the same data for accurate reporting
- Identifying when a recall is issued and which hospital departments are to be alerted. Recall notifications are often spotty and lack important information. Notifications are not distributed to the correct person or teams of people for full visibility and timely compliance.
- Coordinating a recall plan among a diverse group of stakeholders, including Contracting / Sourcing, Supply Chain, Health Information Management, Compliance, Risk Management / Patient Safety, Finance, Revenue Cycle and Accounts Payable, and Information Technology
The challenging realities that are holding you back
While the importance of a strong implant recall management process is obvious, many hospitals find themselves at a deficit when it comes to having the proper tools to implement a reliable process. Limited technologies exist to alert hospitals of recalled items and all fall short of identifying the patient – by name -- where recalled medical devices were used or implanted. At best, hospitals can only pull recalled inventory from their shelves. They are unable to identify patients impacted and notify all involved.
Bandwidth is limited
Hospitals simply do not have the available staff to proactively monitor recalls and do the detailed research to identify past cases. Mobilizing all the hospital stakeholders required to act once a recall is issued can be challenging as it is not always clear what is required of them. The result is that important steps are missed. In the case of the OIG (Office of Inspector General) audit, most hospitals either did not understand their obligations or they failed to act, leading to the potential for fines, penalties, even greater OIG scrutiny, and even potential loss of CMS reimbursement.
Recall information is delayed and incomplete
While the hospital struggles to have the sufficient staff to manage these recalls, they are even further impacted by how the recalls are initially reported.
Responsibility for reporting recalls to hospitals fall to the manufacturer. When a recall is reported to the hospital, it is often sent directly to a contact in biomedical engineering, risk management, or supply chain, which can add even further delays in communicating this information to the person or team that is responsible for managing recalls. The obvious first step for any hospital is to ensure that notification of recalled items are routed to the appropriate person or team in a timely manner.
Missing information can lead to further problems. Key information such as date ranges, item numbers, or lot numbers have been known to be missing from recall notifications.
Specialized knowledge is needed
Medical recalls can be complex and require familiarity with regulations from multiple entities, such as the OIG, CMS, Food and Drug Administration (FDA), and the Office of the National Coordinator of Health Information Technology (ONC). It is imperative for healthcare providers and institutions to be familiar with the regulations and requirements for final consignees.
Recall information is available without charge from online data repositories and third-party subscription services. Some services only send an alert if the recalled item has purchase order history and likely lack the ability to identify historic usage. Whether a free or paid source, the recall data lacks specific information needed to identify variants or recalled devices and is frequently formatted differently than hospital data, making matching a tedious or impossible process.
Tips for a successful implant recall management process
While the perfect recall management process may take time to craft, here are four takeaways to put you well ahead of the curve.
Designate a central contact that can act swiftly and delegate
The success of the process hinges on assigning a central point of contact for receipt of recall notifications. In addition to the responsibility, this persona should also have the authority to initiate the required actions and delegate tasks. With this person in place, you will reduce communication delays and improve the response time in submitting the required form to the recall initiating manufacturer or vendor.
Immediately communicate the contact information of the designated person to all device manufacturers.
Assemble your Implant Recall Team, assign responsibilities, and set response goals
A team comprised of stakeholders from each impacted department should be formed. Examples would be representatives from supply chain, risk management, revenue cycle, health information management, patient safety, and clinical areas. The team members should each possess knowledge of or contacts within the regulatory bodies that monitor recalls, such as the FDA, OIG, CMS, and ONC.
The implant recall team should author, manage and execute the process when a recall is issued. This should include distribution of the recall to all department heads, supply chain leadership, and clinical leads. Further, the team takes action to quarantine any recalled items, collaborate with supply chain IT and data analytics teams to identify historic usage and other pertinent matters.
All departments should have clear direction on their responsibilities when a recall notification is received. In addition, goals and KPIs for timeliness of response should be established to create a clear expectation for your facility’s standards.
Discover usage and existing inventory (notify and sequester)
When the recall is received and interpreted, the most important step is discovering product usage and existing inventory.
We recommend a “Notify and Sequester” approach. This includes notifying impacted patients, as necessary, and sequester existing unused product currently in inventory. A combination of ERP analysis combined with medical records may be required to determine impacted patients and episodes of care. If you do not have ready access to the patients impacted by a recall, this is a good indication that you may not be capturing the data in in the operating room, as required by ONC regulations. For the sake of your patient’s safety, consider improving your data capture processes and technologies so that product recalls do not lead to adverse events. Some recalls can contain hundreds or thousands of serial and lot number combinations and this can be a tedious, yet important task.
Collaborate with finance and accounts payable to address credits
The OIG investigation focused solely on manufacturer credits that were not properly reported to CMS, resulting in overpayment. To keep your facility off of the OIG’s radar, it is important to enlist the finance, revenue cycle, compliance, and managed care teams into the recall process.
The goal is to determine the following:
- Did the facility receive a manufacturer or vendor credit for the product(s) already purchased by the facility, used on / implanted into a patient and identified on the recall notice?
- Did the patient exposure result in a warrant or credit to the patient payor for exposure to the product(s) identified on the recall notice?
The best implant recall management process checks all these boxes
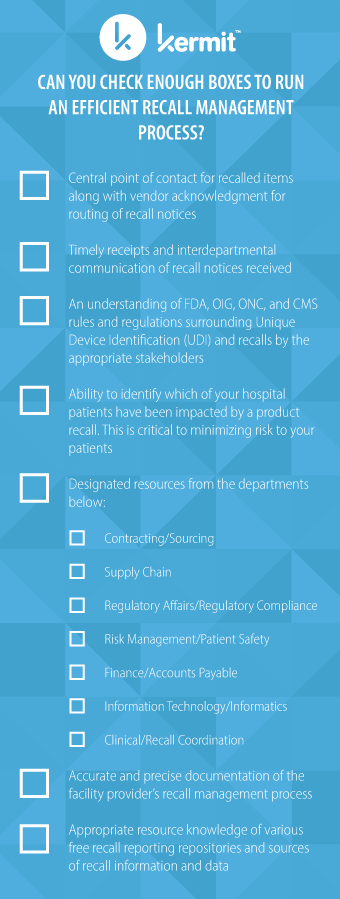
Take inventory of your facilities capabilities to determine if you can check enough boxes to run an efficient implant recall management process:
- Central point of contact for recalled items along with vendor acknowledgment for routing of recall notices
- Timely receipts and interdepartmental communication of recall notices received
- An understanding of FDA, OIG, ONC, and CMS rules and regulations surrounding Unique Device Identification (UDI) and recalls by the appropriate stakeholders
- Ability to identify which patients have been impacted by a product recall. This is critical to minimizing patient risk
- Designated resources in:
- Contracting/Sourcing
- Supply Chain
- Regulatory Affairs/Regulatory Compliance
- Risk Management/Patient Safety
- Finance/Accounts Payable
- Information Technology/Informatics
- Clinical/Recall Coordination
- Accurate and precise documentation of your recall management process
- Awareness and a working knowledge of the free recall reporting repositories and sources of recall information and data
Let Kermit check all the boxes for your facility
Kermit’s Recall Tracking module not only actively reports product recalls, but also tracks the patients who have these devices implanted. For example, Kermit provided a list of patients impacted by a Class I recall of ICD and CRT-D devices for premature battery depletion to its hospital clients within minutes of the recall being published.
Kermit’s recall module combines real-time feeds from the FDA recall database with Kermit’s digitized implant case history and can parse complex combinations of manufacturer part numbers with ranges of lot and serial numbers to pinpoint the recalled items. Kermit pairs its powerful technology with subject matter experts to review, inform and present data to hospital supply chain and risk management teams.
Want to learn more about how you can leverage Kermit’s bill-only solution and the associated recall module? Fill out the form below to get one-on-one consultation and learn more about the Kermit software and services.

