Former medical device sales executives leak industry secrets with their proven and unique way of wringing waste, fraud and abuse from physician preference items.
Implantable medical devices (also known as Physician Preference Items or “PPI”) represent one of the highest supply spend categories for hospitals and health systems, typically exceeding $100 million or more at medium to larger-sized health systems. The top medical device suppliers have distinct advantages in the way they sell, price and invoice for their products. If you and your executive team were to design a process for this spend category today, it would not include products with no price tag on their packaging, unprecedented access by the salesperson to your surgeons and your purchasing department or a paper-based invoicing process with handwritten prices. And yet, that is exactly where we are today. This process has hospitals wasting valuable staff resources chasing down suppliers for corrected invoices and missing valuable insights locked away in paper bills. Based on the work that we have completed in this area, an average of 30% can be saved rather quickly.
Quickly, though, does not mean easy. Your opponent is experienced, nimble, and well-funded. The good news is that there are proven methods to reduce spending on medical implants with the right approach. However, to better understand these approaches, you must first understand what you are up against.
How Medical Device Vendors Maintain Their Leverage
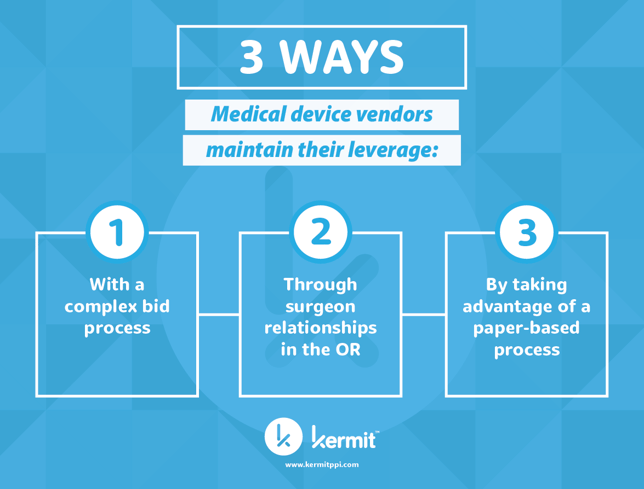
Whether at the negotiation table or in your operating rooms, medical device suppliers exert tremendous leverage over your hospital. Your device vendors employ time-tested methods to control which devices your surgeons utilize and the price you ultimately pay for them.
Here are three advantages that medical device firms employ:
Advantage #1: At the Negotiation Table
Your suppliers know that they hold significant leverage when a contract goes out to bid. With thousands of complex medical devices in any one clinical category, it is unrealistic to expect inhouse procurement teams to understand the device’s technical complexities or whether it is truly unique, as their marketing materials state. The RFP process itself puts hospitals at a disadvantage as supply chain teams need to deal with multiple vendors issuing multiple rounds of unwieldy pricing files each with tens of thousands of line-item entries.
With no objective way to benchmark pricing (FYI: your GPO is not objective, nor are they a fiduciary to you, having financial incentive to keep prices higher than they should be) your hospital is at a tremendous information disadvantage. The result is that you pay higher prices than you need to.
Suppliers are keenly aware that price benchmarking data is readily available to any hospital. Being armed with this data, even if it is accurate, is not enough to obtain the pricing you deserve. Remember the days when it took a PhD to negotiate the best deal on a car? Today, the pricing is far more transparent and yet, people are not confidently walking into auto dealerships. Industries, and particularly their suppliers, adapt quickly to survive.
Advantage #2: In Your Operating Rooms
Medical device representatives leverage entrenched relationships with your surgeons as well as their presence in your operating rooms to influence the day-to-day usage of their products. They know how to subvert your negotiated discounts with proven techniques to increase their price tag. The best intentions of a shrewd supply chain can be quickly unraveled with one interoperative suggestion by the sales professional to the surgeon to use a different implant, and poof! There go your carefully crafted contract terms and cost controls. Sometimes, these item substitutes are in the best interest of patient care; and many times, they are new devices or items which have not been previously contracted. Without the proper oversight and controls, your negotiated pricing is in jeopardy every time a medical device representative enters your O.R.
Advantage #3: The Paper Bill Sheet Process
Finally, this entire transaction is managed through an arcane process where complex medical devices and their component parts are accounted for on paper bill sheets, filled out by medical device reps, and with only a cursory review for accuracy before payment. Critical details about the type of surgery performed and the medical devices utilized are often lost in the translation from paper bill-sheets into enterprise purchasing systems that are not designed to manage this complex spend category. While the purchasing system holds the price, the electronic medical record holds valuable surgical data. It is a tedious process to bring multiple data sets together and few hospitals do so. As a result, off-contract devices slip through, capitated constructs are broken, and hospitals are on the hook for wasted items (with little recourse).
What Can Hospitals Do to Level the Playing Field?
With the suppliers having the advantage, it is easy to see why hospitals struggle to manage this spend category (and why medical device firms generate so much profit). The good news is that there are proven methodologies hospitals can follow that produce savings and ensure sustained spend management.
The lack of visibility for surgeons, supply chain staff and finance executives prevents effective collaboration to reduce costs and manage spend.
If you are ready to change that, consider your answers to these important questions:
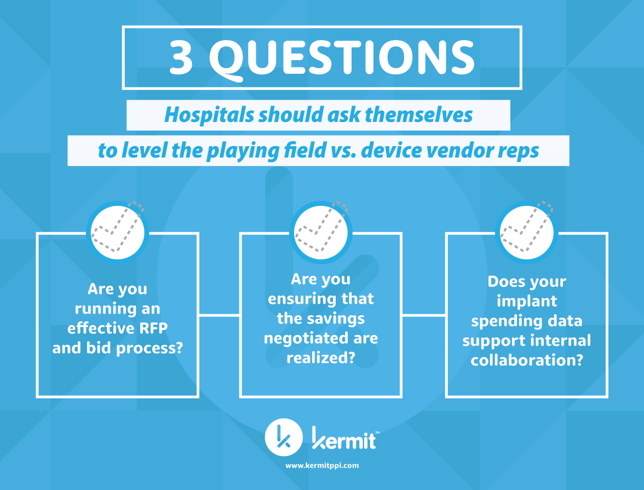
1. Are you running an effective RFP and bid process?
Surgeon input and alignment with administrative objectives must be the first step in an effective bid process. Too often, hospitals consider implant renegotiation a supply chain effort and bring surgeons in when things get desperate. We have seen this happen firsthand with the “suit & tie” wearing consulting firms. Understanding the perspectives of your surgical teams is critical to showing a united front and ensuring that your vendors don’t drive a wedge between the you and your medical staff.
Maintaining the advantage as the buyer in the bid process also involves having a strong, multifaceted team running the process. A “good cop”, a “bad cop” and an “Excel whiz” are all important players who must be dedicated to the process. Suppliers are planning on confusing your supply chain with multiple bid rounds and offers hoping to win a war of attrition where everyone is too fatigued to continue the process for the original stated objective. Suppliers are hoping everyone says, “12% savings is good enough – let’s move on." However, suppliers are not expecting fast, efficient, and accurate analysis of their offers turned back to them with deadlines. Changing the paradigm returns the balance of power back to you. Strong, well-supported, and expedited counter responses from hospitals are paramount to an effective bid.
2. Are you ensuring that the savings negotiated are realized?
Your medical device reps have a thousand-and-one ways to subvert the pricing discounts you just secured in your last round of negotiations. Some protections can be built into your contracts, but sophisticated contracting terms are nearly impossible to enforce with a commission-driven supplier in control of a paper-based process. Consider digitizing and automating the bill sheets, then ensure that each case is audited against your contract terms, pricing, and capitated pricing constructs for accuracy. A rules-based, automated application can create the compliance you need and free valuable staff to perform other duties.
3. Does your implant spending data support internal collaboration?
Consider how your implant data is being stored. Is it accurate and detailed enough to have meaningful conversations with your surgeons about their outlier spending and utilization patterns? Can you track wasted items by surgeon and device rep? Can you compare costs across comparable devices offered from different vendors? Consider a platform that will house implant, spending and procedure data at a level of specificity that supports meaningful analysis and collaboration. The platform should be able to recall accurate cost AND surgical case data with a click.
While those approaches are easy to describe, they are major operational projects that take time, staff, and sometimes other resources. And with the complex category of physician preference, it also can require advanced knowledge of products and an understanding of the vendor-hospital dynamic.
How Kermit Has Helped Hospitals Save More than $150M in PPI Spend
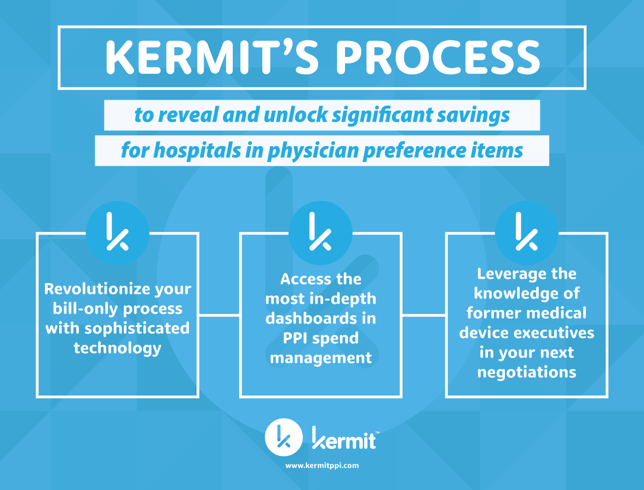
Kermit has served as an advocate exclusively for hospitals in their efforts to manage this spend category more effectively. Our clients save an average of 30% on their annual PPI spend, resulting in more than $150M in total savings for our clients, all without limiting physician preference.
Working from three main tenants, Kermit has a process to reveal and unlock significant savings for any hospital.
1. Revolutionize Your Bill-Only Process with Sophisticated Technology
Capture in-depth device procedure and utilization data along with an image of the supplier’s bill sheet without disrupting the flow in your operating room using Kermit Transact. Kermit’s AI technology flags potentially non-compliant cases and routes them to a PPI expert to ensure cases are paid according to your contract terms with the vendor. Case details are digitized for easy recall and become actionable analytics in the Kermit Insight platform.
2. Access the Most In-Depth Dashboards in PPI Spend Management
Once your bill-sheet data is digitized with your case and procedure data classified, Kermit provides pre-built dashboards to help you track case costs, monitor utilization, manage supplier behavior, visualize wasted item trends, and more. Kermit Insight gives hospital users the ability to drill down into specific data points along with the flexibility to build complex data visualizations to fit their specific needs. For example, combined with Kermit’s proprietary classification system, Kermit Insight allows users to compare specific and detailed surgery types on a surgeon-by-surgeon level to understand cost variations.
3. Leverage the Knowledge of Former Medical Device Executives in Your Next Negotiation
With a proprietary classification system, best-in-class benchmarking, an ear to the rail of the latest in product advancement and supplier strategies, and years of experience in physician preference from a team of strategic advisors, Kermit has the pedigree and knowledge to fully manage your PPI negotiations from start to finish in 22 different surgical categories. Our flexible and proven project-driven approach support your existing supply chain team. We save our clients an average of 30% on their PPI spend with no-risk options that include use of the complete Kermit application at no additional cost.
Want to Learn How Kermit Can Permanently Change the Game for You?
Kermit has experience working with highly-varied environments from rural hospitals, community and regional medical centers, academic health systems and large integrated delivery networks. Learn how we can tailor our approach to you. Fill out of the contact form below to learn more.

